5 points’ summary of uterine fibroid (leiomyoma)
What is uterine fibroid?
- Uterine fibroid is a non-cancerous growth (benign tumour) from the wall of the uterus. The medical term is ‘leiomyoma’
- It can be singular or multiple in one individual
- The size can vary from < 1 cm to over 20 cm or even bigger
- Uterine fibroid is very common, especially for women from their 40’s onwards
- The risk factors of having uterine fibroid include: family history of fibroid, obesity, no history of pregnancy, diet with high content of red meat and high blood pressure
- Uterine fibroids will regress after menopause or in the absence of oestrogen
What symptoms do uterine fibroid(s) cause?
Most uterine fibroids are incidental findings on check-up and do not cause any symptoms. However, some women do have symptoms, with varying degrees of severity, such as:
- Menorrhagia (heavy menstruation)
- Painful period
- Pressure symptoms within the tummy
- Urinary symptoms such as frequency of urine or bladder retention
- Subfertility or pregnancy complications
How is uterine fibroid diagnosed?
- Ultrasound – adequate in establishing the diagnosis, lower cost
- MRI – accurately characterize the pelvic masses, but at a higher cost
When is treatment indicated for uterine fibroids?
- Heavy menstruation causing anaemia
- Rapid increase in size
- Pressure or urinary symptoms
- Subfertility or pregnancy complications
- Diagnosis of benign lesion not certain
What are the treatment options of uterine fibroid(s) if indicated?
- Myomectomy – remove the fibroid(s) and conserve the uterus, which can be performed via laparotomy or laparoscopic approaches
- Hysterectomy – remove the whole uterus, which can be performed by laparotomy, laparoscopic and vaginal approaches
- Hysteroscopic myomectomy – remove the fibroid(s) via vagina and cervix; only for small submucosal fibroids
- High Intensity Focused Ultrasound (HIFU) – Special machine to emit focused high energy at the lesions to ablate the pathology
- Uterine artery embolization (UAE) – reducing blood supply to the uterus will cut down blood supply to the fibroid, thereby may cause necrosis of the fibroid tissue
Uterine fibroid (leiomyoma) – Full article
1. What is uterine fibroid?
- Uterine fibroid is a non-cancerous growth (benign tumour) from the wall of the uterus. The medical term is called ‘leiomyoma’. It is made up of smooth muscle cells and fibrous connective tissue.
- It can be singular or multiple in one individual.
- The size vary from < 1 cm to over 20 cm or even bigger.
- Uterine fibroid is very common, especially for women in their 40’s. It is estimated that 1 in 3 women will have uterine fibroid(s) at some point of their life.
- The cause of uterine fibroid is still unknown. The risk factors include: family history of fibroid(s), obesity, no history of pregnancy, diet with high content of red meat, high blood pressure.
- Uterine fibroids will regress after menopause or in the absence of oestrogen.

2. Different types of uterine fibroids
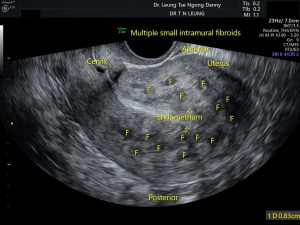
Uterine fibroids are named based on the location of the mass in the uterus (see picture):

- Intramural fibroid
(i) Intramural fibroid is located in the muscular wall of the uterus.
(ii) It is the most common type.
(iii) Depending on the size, it can cause distortion of the uterus and symptoms.
- Subserosal fibroid
(i) Subserosal fibroid grows from the muscular wall outwards.
(ii) Small subserosal fibroid does not cause any problem.
(iii) Large subserosal fibroid may press on the adjacent organs such as bladder or bowels causing symptoms.
- Submucosal fibroid
(i) Submucosal fibroid grows inward and protrudes into the uterine cavity.
(ii) While it is not as common compared with the other types, it is more likely to cause menstrual symptoms due to its location.
(iii) Without treatment, it may increase the risks of pregnancy complications.
- Pedunculated fibroid
(i) Pedunculated fibroid is one that is attached to the uterus by a stalk.
(ii) It can grow outside the uterus or within the uterine cavity.
3. Symptoms of uterine fibroid(s)
Most uterine fibroids are incidental findings on check-up and do not cause any symptoms. However, some women do have symptoms, with varying degrees of severity:
- Menorrhagia (heavy menstruation)
- Painful period
- Pressure symptoms within the tummy
- Urinary symptoms such as frequency of urine or bladder retention
- Subfertility or pregnancy complications
During pregnancy, the fibroids will grow in size and occasionally will develop red degeneration. After delivery, they will shrink in size. (see the section on uterine fibroid(s) in pregnancy)
4. Diagnosis of uterine fibroid(s)
- Ultrasound
In majority of cases, ultrasound is adequate in establishing the diagnosis. However, at times, there may be atypical features of an uterine mass, in which case, other imaging techniques might be required.
- MRI
(i) MRI can accurately characterize pelvic masses. It has been shown to be more sensitive in identifying uterine fibroids than ultrasound.
(ii) Like ultrasound, it does not have irradiation.
(iii) MRI is more costly compared with ultrasound and hence it is not employed as the first-line imaging technique.
- Differentiation from leiomyosarcoma (malignant uterine tumour)
(i) When an uterine mass is identified, it is important to determine whether it is a fibroid (benign) or a malignant lesion (such as leiomyosarcoma).
(ii) The incidence of leiomyosarcoma is very very low, estimated to be only 0.35-0.64 per 100,000 women.
(iii) The chance of a fibroid turning into leiomyosarcoma is estimated to be only in the order of 1 in 500-700.
(iv) Features suggestive of malignant mass include (a) a history of rapid increase in size; (b) increase in vascularity on colour doppler ultrasound scan; (c) suspicious MRI features; (d) significant increase in lactate dehydrogenase level in blood.
5. When is treatment indicated for uterine fibroids?
The indications include:
- Heavy menstruation causing anaemia
- Rapid increase in size
- Pressure or urinary symptoms
- Subfertility or pregnancy complications
- Diagnosis of benign lesion not certain
6. Treatment options of uterine fibroid(s)
- Myomectomy
(i) It is an operation to remove the fibroid(s) and conserve the uterus.
(ii) This operation can be performed via laparotomy and laparoscopic approaches.
(iii) In the laparotomy approach, the fibroid(s) are removed via an open wound in the tummy. This approach is suitable for very big fibroids and conditions where the laparoscopic approach is not suitable.
(iv) The laparoscopic approach is the most frequent way of myomectomy nowadays. Usually 3 small skin incisions are made. The fibroid(s) are removed from the uterus via these incisions and the uterine wounds are sutured. The fibroid(s) are then morcellated into small chips before they are removed through one of the skin incisions (see photo). In general, this approach is associated with less post-operative wound pain and quicker recovery time compared with the laparotomy approach.

(v) Like all other surgeries, myomectomy also carries some operative risks although infrequent:
a. Infection
b. Excessive bleeding
c. Injury to the adjacent organs such as bowel, bladder, ureters and major vessels
d. Haematoma at the uterine wound
e. Bowel adhesions to the uterine wound
(vi) Following myomectomy, time should be given for the uterine wound to heal completely before attempt of pregnancy. Usually for uncomplicated situation, this period is at least 6 months.
(vii) Recurrence- in general it is estimated to be 15%.
- Hysterectomy
(i) This is an operation to remove the whole uterus.
(ii) Suitable for women who have completed the family.
(iii) It can be performed by laparotomy, laparoscopic and vaginal approaches. Nowadays, the majority of hysterectomy are performed via laparoscopic approach.
(iv) Although infrequent, it carries the following risks:
a. Infection
b. Excessive bleeding
c. Injury to the adjacent organs such as bowel, bladder, ureters and major vessels
d. Haematoma at the ceiling of the vagina
- Hysteroscopic myomectomy
(i) Hysteroscopic approach is only suitable for pedunculated fibroid within the uterine cavity or submucosal fibroid < 3 cm in size. There is no wound in the tummy and the instruments are passed via the vagina and cervix for removal of the fibroid(s). The recovery time is very quick.
(ii) Risks are infrequent but can include infection, excessive bleeding, uterine perforation, damage to the lining of the uterus and incomplete removal of the fibroid(s).
- High Intensity Focused Ultrasound (HIFU)
(i) HIFU is a relatively new treatment modality for benign uterine tumours.
(ii) It is a technology which involves focusing beams of ultrasound wave to one point, typically a small volume of 5 mm in diameter. The intention is to raise the temperature to above 60C for one second or longer in order to cause tissue necrosis. By moving this focus to different parts of the tumour, the majority of the tumour can be destroyed.
(iii) During the ablation process, the HIFU beam has to be targeted and monitored under image guidance either by MRI or ultrasound.
(iv) The application of this technique under ultrasound guidance (USgHIFU) as treatment of uterine fibroid has been reported in Mainland China since 2002. Since then, USgHIFU has been further developed and is now considered as one of the alternative treatments for fibroids apart from surgery in many parts of China.
(iv) The application of this technique under ultrasound guidance (USgHIFU) as treatment of uterine fibroid has been reported in Mainland China since 2002. Since then, USgHIFU has been further developed and is now considered as one of the alternative treatments for fibroids apart from surgery in many parts of China.
(v) The success rate of HIFU in treatment of fibroid(s) depends on the percentage of the fibroid being destroyed. In general, the fibroid shrinks by 45% at 3 months after treatment and this increases to 60% by 6 months. It is expected that 50% of patients will have improvement of symptoms at 3 months and this will increase to 90% at 6 months.
(vi) HIFU is in general a safe procedure under expertise team. Operative risks are uncommon but can occur. They include skin burn, acute urinary retention, pain at lower spine or legs, nerve and bowel injury.
(vii) Not all women with uterine fibroids will benefit from HIFU treatment. For the location of some fibroids, HIFU may not be possible or can be dangerous Careful pre-operative assessment by ultrasound and MRI is very important for selection of suitable women who will likely benefit from it.
- Uterine artery embolization (UAE)
(i) Fibroid has blood supply from the uterus. Hence, by reducing blood supply to the uterus will cut down blood supply to the fibroid, thereby may cause necrosis of the fibroid tissue.
(ii) This procedure is performed by radiologists under local anaesthesia. A catheter is passed from a major artery in the groin of the woman into the circulation system. Eventually this catheter is thread into the artery supplying the uterus. Small particles will be injected through the catheter into the blood vessels that supply the fibroid(s) to block the blood supply.
(iii) UAE will be performed in both the left and right uterine arteries.
(iv) For control of symptom of heavy menstrual bleeding, it has been reported to result in improvement of symptoms in 60% of cases.
(v) It might not be very effective for large fibroids or those women with a large number of fibroids. It is not suitable for pedunculated fibroids.
(vi) UAE is in general a safe procedure under expertise radiologists. Operative risks are uncommon but can occur. They include bleeding, infection, bruising at groin, injury to the arterial system during the insertion of the catheter, pelvic pain and early menopause due to diminished blood supply to the uterus.
(vii) Those who wish to become pregnant in the future would not be recommended to have this procedure.