1. Identical twins versus non-identical twins
- Identical twins are named ‘monozygotic twins’ in medical term. They result from fertilization of one egg by one sperm to form one zygote which then splits into 2 embryos.
- Non-identical twins are named ‘dizygotic twins’ in medical term. They happen when 2 separate eggs are fertilised by 2 sperms to form 2 embryos. They are just like 2 siblings and hence they are also called ‘fraternal’ twins.
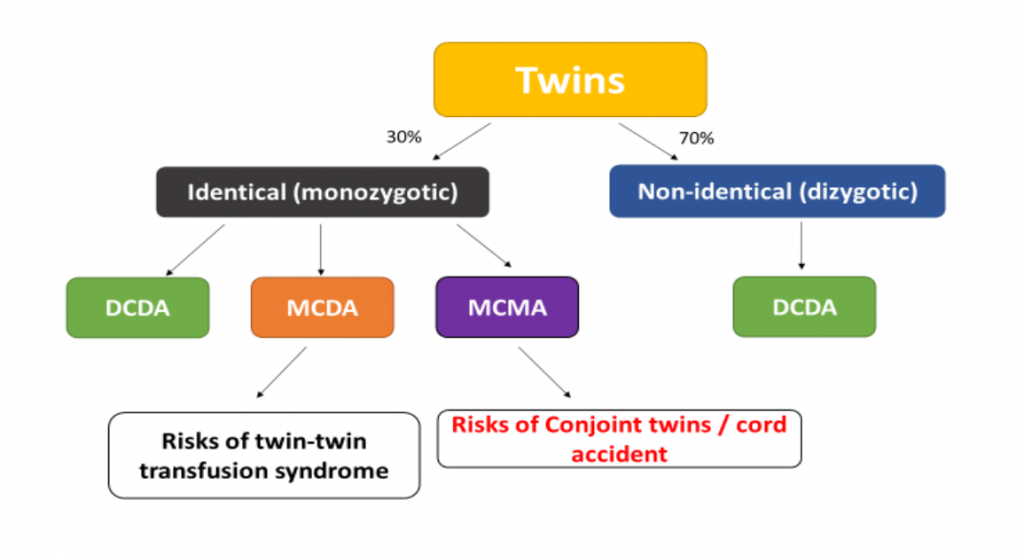
- Non-identical (dizygotic) twins are far more common than identical (monozygotic) twins and account for 70% of all twin pregnancies. The frequency of non-identical twins is variable among different populations. However, the frequency of identical twins is globally constant at 3 to 5 per 1,000 births.
- Non-identical twins have 2 separate placentae and each twin has a separate amniotic sac. So, it will always be Dichorionic Diamniotic (DCDA) twins (‘Di’ means ‘two’).
- There are 3 different kinds of identical (monozygotic) twins, depending on the number of placentas:
- (i) Dichorionic Diamniotic (DCDA) twins
- They happen when splitting occurs by 3 days after fertilization. They occur in ~25% of all identical twins. This form of twins bears the least risks during pregnancy as each fetus has its own placenta, and the fetuses are separated by the amniotic membrane.
- (ii) Monochorionic Diamniotic (MCDA) twins
- ‘Mono’ means ‘one’. There is only one placenta or that the two placentae are connected. The fetuses are separated by the amniotic membranes. They occur when splitting occurs at 4-8 days after fertilization. This form constitutes ~70% of all identical twins.
- (iii) Monochorionic Monoamniotic (MCMA) twins
- There is only one shared placenta and no amniotic membrane between the twins. They occur in ~5% of all identical twins. This kind of identical twins happen due to splitting after 9 days following fertilization. The umbilical cord between the fetuses might intertwine with each other. If the splitting occurs >12 days after fertilization, conjoint twins usually result.
2. Clinical classification of twins
- Of clinical relevance, twins are classified into 3 categories by ultrasound:
- (i) DCDA twins
- (ii) MCDA twins and
- (iii) MCMA twins

- For DCDA twins, there are 2 discrete placentae and both twins are separated by the amniotic membranes. They account for the majority of twin pregnancies (~75%). The twins can be non-identical or identical (due to early splitting- see above).
- For MC twins, there is only one placenta or the two placentae are joined together. Vascular communication is found between the two share of the placentae. This kind of twins must be identical ones. They are further classified into MCDA twining if the twins are separated by amniotic membranes, or MCMA if the fetuses are not separated by amniotic membranes. MCMA twins are very rare, accounting for ~1% of all twin pregnancies.
- The risks are higher with MC twin pregnancies due to the sharing of blood supply in the placentae (see the section on risks of monochorionic twin pregnancies).
- The determination of the chorionicity is therefore clinically more important compared with knowing the zygosity (i.e. whether it is identical or non-identical).
3. Ultrasound diagnosis of twin pregnancy
- Twin pregnancy should be diagnosed by ultrasound.
- The chorionicity can be accurately determined at 6-9 weeks of gestation. If two separate gestational sacs are seen, dichorionic (DCDA) twins are diagnosed. If only one gestational sac is seen and 2 fetal poles are noted within that sac, it is monochorionic (MC) twins. The amniotic sac might not be too obvious at early gestation. Hence, while MC twins can be accurately diagnosed in early gestation, the differentiation of MCDA or MCMA might have to be determined in later stage. One important clue is the number of yolk sac seen on ultrasound. If there are two yolk sacs, it should be MCDA twins. If only one yolk sac is seen, it should be MCMA twins.
- At 10-13 weeks of gestation, even there are two gestational sacs, they would join together. The determination of chorionicity will depend on the number of placental mass and the characteristic intertwin membrane-placental junction. It has been shown that the accuracy on chorionicity is 100% before 14 weeks of gestation. After 14 weeks, the accuracy might drop. The amniotic membranes can be reliably seen at this gestation. Hence, in the case of MC twins, it is possible to accurately determine whether it is MCDA or MCMA twins.
- Most units offer closer ultrasound intervals for MC twin pregnancies between 16-28 weeks of gestation to look out for complications such as twin-twin transfusion syndrome (see the section on risks of monochorionic twin pregnancies).
- Making the diagnosis of twin pregnancy is not good enough. It is important for obstetricians or sonographers to differentiate whether it is DCDA, MCDA or MCMA twin pregnancies.