Pre-eclampsia is a complication of pregnancy which is characterized by hypertension and protein in urine. It usually occurs in the second half of the pregnancy. The incidence around 2% in Hong Kong. Severe pre-eclampsia is a dangerous and potentially life threatening.
1. Diagnosis
- Elevated blood pressure
- (i) In women with previously normal blood pressure, blood pressure ≥140 mmHg systolic or ≥90 mmHg diastolic on 2 occasions taken at least 4-6 hours apart after 20 weeks’ gestation.
- (ii) In a woman with pre-existing hypertension before 20 weeks’ gestation, an increase in systolic blood pressure of ≥30 mmHg or an increase in diastolic blood pressure of ≥15 mmHg.
- Proteinuria: ≥ 0.3 grams (300 mg) of protein in a 24-hour urine sample or a spot urinary protein to creatinine ratio ≥0.3.
2. Potential risks
- The mother’s risks
Pre-eclampsia is more than just a combination of high blood pressure and protein in urine. It is a disorder affecting different systems of the pregnant women and may lead to the following complications:
- (i) Eclampsia (generalized convulsion)- generalized convulsion caused by pre-eclampsia is called ‘eclampsia’. It presents serious risks to both the mother and the unborn baby.
- (ii) Clotting system- severe pre-eclampsia can lead to low platelet count and disorder of the coagulation system, which in turn can lead to bleeding tendency and failure of clotting with the wounds.
- (iii) Renal (kidney) system – the kidney function can deteriorate and in severe cases, it can lead to complete loss of kidney function.
- (iv) Hepatic (liver) system – there might be damage of the liver leading to liver failure.
- (v) Cardiovascular system – there are risks of stroke, heart failure and oedema with the lung in severe pre-eclampsia.
- The baby’s risks
Pre-eclampsia also poses significant risks to the unborn child especially if the mother’s condition is not stable.
- (i) Intrauterine fetal growth restriction – the placental function might be impaired, which in turn leads to reduction in amniotic fluid volume and intrauterine fetal growth restriction.
- (ii) Placental abruption – severe pre-eclampsia is associated with separation of placenta from the uterine wall, a condition called ‘placental abruption’. The blood supply to the baby will be impaired or stopped in such case, leading to in-utero asphyxia or fetal death.
- (iii) Preterm delivery – delivery is the only effective cure of severe pre-eclampsia. Therefore, if severe pre-eclampsia is developed before 34 weeks, preterm delivery to save the mother put the baby at risks of those complications related to early preterm delivery.
- (iv) Intrauterine fetal death – related to severe placental insufficiency and/or placental abruption.
3. Clinical features
Most affected women will have no symptom. Hence it is important to have regular blood pressure measurement and urine test for protein at antenatal check-up. Those with significant protein in the urine might have very significant swelling with the ankles (called ankle oedema). However, ankle oedema is not very specific to pre-eclampsia and can also occur in normal pregnant women.
For women with severe pre-eclampsia with a high chance to develop into eclampsia, the following conditions may appear:
- headache
- blurring of vision
- pain over stomach or right side of tummy
- vomiting
- low urine output
- brisk jerks on examination by doctor (hyper-reflexia)
4. Management
Delivery of the baby and the placenta is the only cure for pre-eclampsia. If pre-eclampsia has developed in preterm gestation, especially < 34 weeks, a balance has to be made between the risks of continuation of pregnancy (i.e. further deterioration of the condition) and the risks of preterm delivery for the baby.
The main aims of the management are:
- Protect mother from complications of severe pre-eclampsia.
- Minimize the risk to unborn baby.
- Deliver the baby when the risks of continuation of pregnancy > risks of prematurity.
5. Screening for pre-eclampsia
- Predictive factors for pre-clampsia
- (i) Maternal factors
- Various factors related to the pregnant women and their families are found to be associated with the development of pre-eclampsia, including the first pregnancy, older age and higher weight, medical diseases such as chronic hypertension and kidney diseases, personal history of pre-eclampsia in previous pregnancies and family history of pre-eclampsia. The limitation of using these factors alone is that the majority of pregnancies with pre-eclampsia do not have any risk factors apart from being the first pregnancy.
- (ii) Mean arterial blood pressure (MAP)
- The use of mean blood pressure (2/3 diastolic blood pressure + 1/3 systolic blood pressure) in early pregnancy has been shown to be more useful than the measurement of either systolic or diastolic blood pressure for prediction of subsequent development of pre-eclampsia.
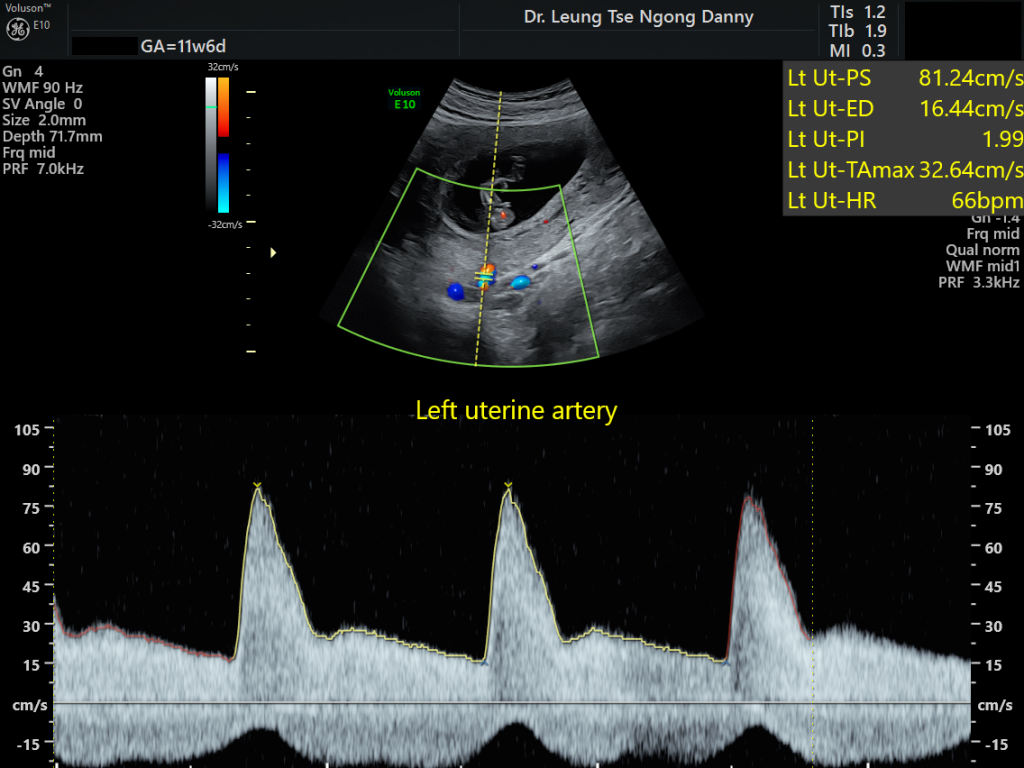
- (iii) Uterine artery doppler of the mother (UA doppler)
- Research has discovered that the ultrasound measurement of the uterine arteries of the pregnant women is useful for identification of women at high risks for pre-eclampsia. This can be measured in the first trimester between 11-13 weeks of gestation. A high PI value of the uterine artery doppler is associated with a higher chance of developing pre-eclampsia subsequently.
- (iv) Mother’s blood
- A protein in the mother’s blood called Placental Growth Factor (PLGF) is produced by the placenta. For those pregnancies which will develop pre-eclampsia subsequently, the level of PLGF in early pregnancy will be much lower.
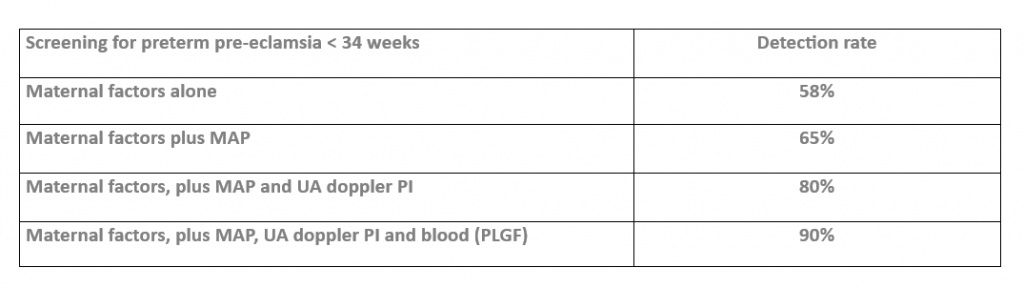
- Strategies of screening for pre-clampsia in early pregnancy
Research has established robust algorithms to screen for subsequent development of pre-eclampsia from assessment in the early pregnancy between 11-13 weeks of gestation, using a combination of the predictive factors. The benefit of screening early is that it allows more time for preventive measure to be instituted if a woman is found to be of high risk. This provides a higher chance of effective prevention.
- Effective preventive measures
In a large clinical study published in 2017, the use of low dose aspirin 150 mg daily from 11-14 weeks of gestation can reduce the chance of developing pre-eclampsia < 34 weeks of gestation by 80%. Further research analysis has shown that aspirin is useful only when it is initiated at ≤16 weeks of gestation and at a daily dose of ≥100 mg. This is the reason why screening for pre-eclampsia should be arranged between 11-13 weeks of gestation.
6. Conclusion
Pre-eclampsia is a disorder of pregnancy which carries significant risks to both the mother and the babies. Now there is an effective screening program between 11-13 weeks of gestation, with the use of maternal factors, mean arterial blood pressure, ultrasound measurement of UA PI and the measurement of PLGF in the mother’s blood. It is also proven that high-risk pregnant women can benefit from having low dose aspirin for prevention of the development of pre-eclampsia subsequently.
References:
1. Ronik DL, et al. Aspirin versus placebo in pregnancies at high risk for preterm pre-eclampsia. New England J Med 2017;377(7): 612-622.
2. Roberge S, et al. Aspirin for prevention of preterm and term pre-eclampsia: systemic review and metaanalysis. Am J Obstet Gynecol 2018;218(3):287-293.
